
9 min read
Value-Based Purchasing in Healthcare Explained
Value-based purchasing is a healthcare payment model that incentivizes high-quality care. Learn the key benefits and how healthcare systems might incorporate this practice.
Healthcare revolves around achieving positive outcomes and safe treatment options for patients. However, certain healthcare delivery models don’t always prioritize these vital aspects, especially considering the ever-increasing costs of healthcare services.
Yet there’s a proactive approach that addresses the high cost of healthcare: value-based purchasing (VBP). VBP also improves patient satisfaction by fostering greater collaboration among healthcare providers and making the patient experience one of the key evaluation metrics for hospitals. Discover what it entails, how it operates, and best practices to optimize its implementation.
Keep reading to learn:
- Value-based purchasing definition, history, and benefits
- How value-based purchasing works
- Ways to smoothly incorporate value-based purchasing
- Frequently Asked Questions
Value-based purchasing definition, history, and benefits
Value-based purchasing (VBP) is a healthcare payment model under which healthcare providers are reimbursed based on the quality and value of care rather than solely on the quantity of services provided. By implementing VBP, hospitals can improve the value of healthcare services, reduce costs, and reward the best-performing care providers.
Hospitals typically use the fee-for-service model of healthcare delivery; with it, providers are rewarded based on the volume of services they provide. However, this approach is not super efficient as it tends to focus more on addressing immediate symptoms rather than implementing comprehensive, outcome-driven treatment plans. Thus, it doesn’t provide enough incentive for hospitals to prioritize positive patient outcomes.
For example, let’s say a patient seeks treatment for lower back pain. Under a fee-for-service model, the healthcare provider might order multiple imaging tests, prescribe pain medications, and refer the patient to physical therapy sessions, each resulting in additional payments. Whether or not the back pain goes away, healthcare providers are paid for all diagnostics, tests, consultations, prescriptions, and other provided services. Under the concept of value-based care, the clinic or hospital would be paid according to how well they diagnosed and treated the back pain.
Although VBP and a positive outcome should be considered a priority in most countries, it’s much more common globally for patients, insurance, state healthcare, or any other paying party to pay for each service carried out under the fee-for-service model. In the past 15 or so years, the US, which is known for its complicated and expensive healthcare system, has taken some steps towards value-based purchasing. We can observe American VBP programs as examples of how value-based purchasing can change the healthcare landscape.
The Affordable Care Act (2010) introduced some mandatory value-based purchasing programs for hospitals that accept Medicare. The Centers for Medicare and Medicaid Services (CMS), which provides coverage for people on Medicare plans, has a few VBP programs that apply to various circumstances and medical institutions.
One of these is the Hospital Value-Based Purchasing Program, under which CMS evaluates participating hospitals based on numerous criteria. This U.S. federal agency withholds a portion of Medicare payments from participating hospitals, and these funds are then redistributed based on hospitals’ performance scores.
With its value-based purchasing programs, the CMS hopes to encourage healthcare providers to focus on the end result of treatment, coordinate care, and minimize healthcare expenditures for patients. Even though fee-for-service remains the dominant healthcare payment model in the U.S., where Medicare is concerned, CMS has set a goal to have 100% of all Medicare beneficiaries in a value-based program by 2030.
The Hospital Value-Based Purchasing Program is notable for numerous important benefits:
- Increased transparency of a provider’s quality of care.
- Comprehensive care achieved through better coordination between hospitals and medical professionals.
- Lowered costs as a result of more efficient treatment and elimination of unnecessary procedures.Improved patient experience during hospital stays.
- Promotion of evidence-based care standards and protocols.
Yet attaining these benefits proves challenging for some medical institutions and the VBP system needs further improvements. According to a study published in Front Public Health, American hospitals serving larger segments of disadvantaged populations or complex patients face difficulties in reducing costs while improving care quality and, as a result, face more penalties. Nevertheless, let’s see how the VBP program encourages medical institutions to improve the patient experience.
How value-based purchasing works
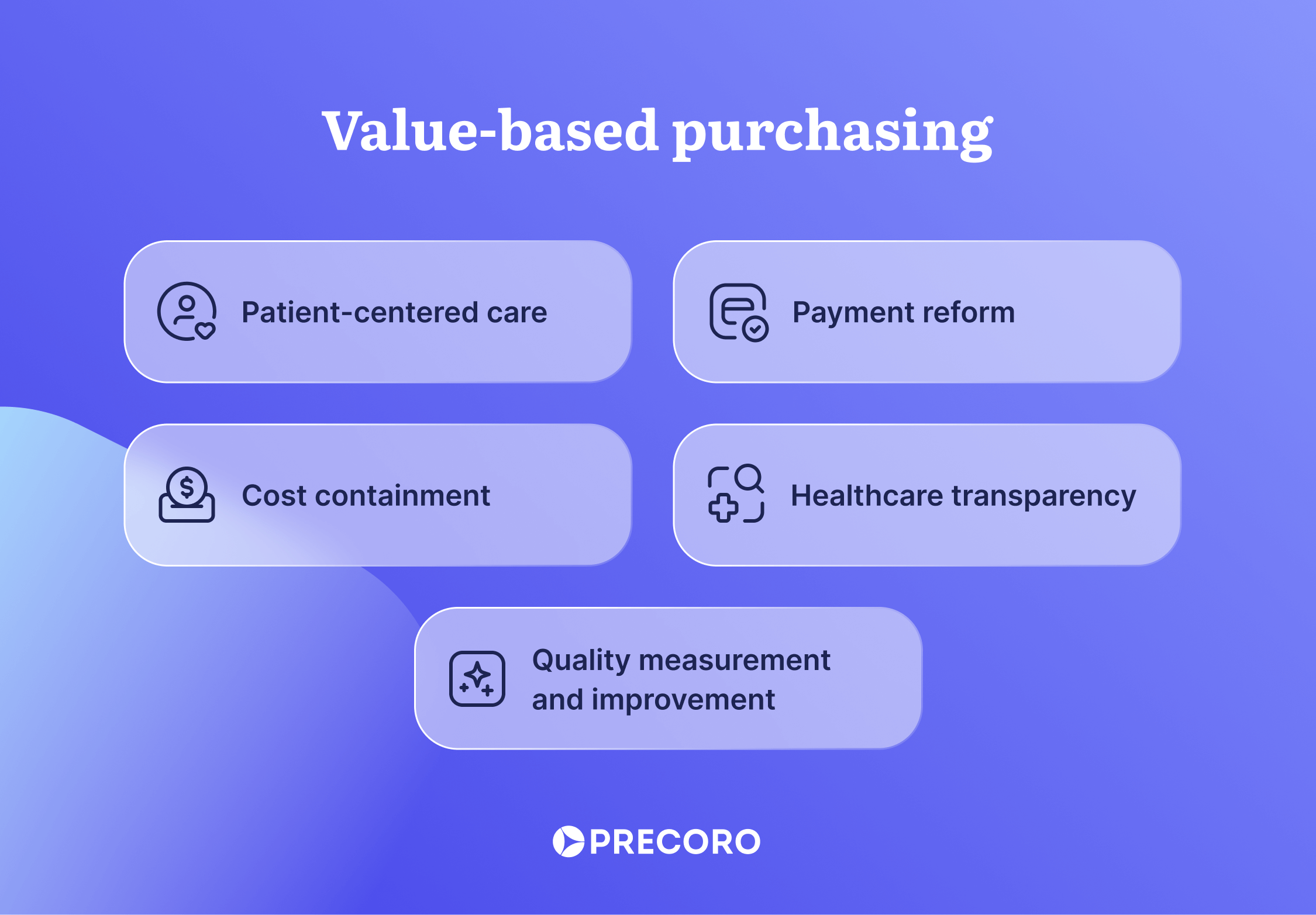
Value-based purchasing encompasses a range of initiatives and strategies aimed at improving the quality and effectiveness of healthcare delivery while controlling costs. Let’s see how these goals can be achieved by taking as an example the Hospital Value-Based Purchasing (HVBP) program implemented by the CMS:
Quality measurement and improvement
Under the HVBP, the CMS assesses hospital performance using quality metrics that include:
- Mortality and complications
- Healthcare-associated infections
- Safety measures
- Patient experience
- Efficiency and cost reduction in care delivery
The Centers for Medicare and Medicaid Services agency assigns hospitals two scores for each factor that is measured. The first score is based on how well they perform in an area against other hospitals, and the second score is determined based on how much they have improved compared to a prior period. The final score on each measure is the higher of the two scores, and Medicare payments are adjusted according to the hospital’s overall performance in all areas.
Payment reform
Providers are incentivized via financial rewards or penalties to improve performance on the above-mentioned metrics. The VBP program adjusts payments to hospitals under the Inpatient Prospective Payment System (IPPS) based on care quality, shifting from volume-based reimbursement to quality-focused models.
It works in the following way: the VBP program withholds a portion of Medicare payments (2%) from participating hospitals. Then, that money is used to fund incentive payments to hospitals based on their performance in the program.
Another emerging reimbursement model gaining traction is the shared savings approach, particularly through bundled payments. In this framework, healthcare providers are allocated a predetermined sum to manage a patient’s treatment, either for a specific ailment or procedure or over a defined timeframe.
Should the provider effectively treat the patient for less than the allocated sum, they become eligible for a portion of the surplus in accordance with their contract terms. Conversely, if the expenses surpass the fixed amount, the provider forfeits the potential reimbursement they might have received under conventional reimbursement models.
Patient-centered care
Healthcare value-based purchasing emphasizes patient-centered care delivery, focusing on improving the overall patient experience and outcomes. This can be achieved through several strategies:
- VBP incentivizes providers to prioritize preventive care measures to reduce the likelihood of disease occurrence or progression.
- Providers involve patients in treatment decisions by discussing various options, risks, and benefits.
- Value-based purchasing encourages seamless coordination among healthcare providers across various settings to ensure continuity of care.
Cost containment
The objective of value-based purchasing is to reduce healthcare expenditures while improving patient outcomes. Approximately 25 percent of healthcare spending in the United States is considered wasteful. To address such waste, providers are encouraged to determine what it actually costs to deliver their services in a way that ensures measurable outcomes for patients. Cost-efficient measures are primarily carried out with the goal of reducing unnecessary utilization of services. For example, the necessary practices might be:
- A reduction in avoidable hospital admissions, readmissions, and multiple diagnostic tests.
- A reduction in hospital cost per day, length of stay, and/or ICU length of stay.
Cost-efficiency in healthcare can be achieved through efficient preventive care, by distributing resources that encourage a healthy lifestyle, and by adding options for care, including post-acute care and telehealth programs. It’s also important for hospitals to efficiently allocate resources and monitor budgets to eliminate unnecessary spending or shortages in critical supplies.
Healthcare transparency
VBP promotes transparency in healthcare by providing access to not just cost information but also provider performance data that describes hospitals participating in the Hospital Value-Based Purchasing Program, namely:
- The hospital’s performance on each measure and the total performance score
- The number of hospitals receiving value-based incentive payments under the
program, including the range and amount of these payments - The number of hospitals receiving less than the maximum value-based incentive payment available for that fiscal year and the range and amount of these payments
This transparency allows patients to make informed decisions about their healthcare options and encourages providers to strive for excellence in care delivery.

Ways to smoothly incorporate value-based purchasing
In order to implement value-based purchasing, hospitals can focus on two key areas: performance on health outcomes and cost management. Finding the right tools proves to be a major help in optimizing these aspects.
Implementing EHR software
Electronic Health Record (EHR) software, also known as Electronic Medical Record (EMR), is a must-have tool for medical institutions. It serves as a secure and reliable database of patients’ medical histories, lab results, prescriptions, and treatments. Such a system helps healthcare providers improve the quality of care delivery in several ways:
- Centralized data allows hospitals to analyze patient populations comprehensively and identify trends, patterns, and areas for improvement in care delivery.
- Healthcare providers can seamlessly share patient data across different departments, specialties, and care settings to avoid the risk of losing or lacking essential patient health data and reduce redundancies in treatment.
- Data analytics and reporting capabilities enable hospitals to generate performance reports and analyze clinical data.
- Patients have complete visibility into their conditions and treatment through access to their health records, lab results, medication lists, and treatment plans.
Adopting a procurement system
Cost-efficiency is an important part of value-based purchasing. However, a hospital that doesn’t have real-time visibility into its expenses, inventory, and supplier performance will struggle to achieve this. Without a comprehensive approach to procurement, medical institutions risk overspending on supplies and services. This can lead to:
- Limited funds for quality improvement investments.
- Diversion of funds from critical areas like staff training, technology upgrades, and patient safety initiatives vital for VBP success.
- Failure to attain positive performance scores on cost-containment measures.
While tracking expenses in spreadsheets may suffice for small companies, it proves inefficient for institutions managing a high volume of purchases. Therefore, when a hospital aims to take spending under complete control and find ways to reduce costs without disrupting operations, procurement software becomes indispensable.
Let’s see how a procurement system like Precoro can assist hospitals:
- Using full visibility into all procurement processes, hospitals can analyze the demand and stay cost-effective by predicting spending, grouping purchases, and negotiating bulk discounts.
- Healthcare institutions can select suppliers through the comprehensive RFP process and quickly onboard them. Moreover, hospitals can assess supplier performance by monitoring whether suppliers fulfill their responsibilities on time and in full.
- Hospitals can set up budgets and monitor expenses in real time, and can track and analyze spending across various departments and procurement categories.
- Centralized information about available supplies and equipment ensures hospitals never experience shortages or buy excess reserves.
Frequently Asked Questions
Value-based purchasing (VBP) is a healthcare payment model where government agencies (i.e. the CMS in the U.S.) or private insurers use incentive payments to reward providers who deliver high-quality care, ensure positive patient outcomes, and do so cost-efficiently.
The focus of pay-for-performance or value-based purchasing systems should be on improving patient outcomes, enhancing quality of care, promoting cost-effectiveness, and encouraging patient satisfaction.
As part of the value-based purchasing program, assessments of care providers typically include evaluations of patient outcomes, safety measures, adherence to clinical guidelines, patient satisfaction scores, and cost efficiency.
Understanding value-based purchasing
The value-based purchasing model represents a shift from the traditional fee-for-service approach, under which healthcare providers are paid based on the volume of services rendered, regardless of the quality or outcomes. The CMS Hospital VBP Program determines reimbursement based on hospital performance on health outcomes, patient safety, patient satisfaction, and cost-effectiveness.
If the hospital achieves high scores compared to other medical institutions and its own historical performance, CMS reimburses it on top of typical fee-for-service payments. Otherwise, CMS penalizes its Medicare revenue. With such a system, the VBP program strives to hold providers accountable for the cost and quality of health care services a person receives.
Value-based purchasing emphasizes preventive care and collaboration among health care providers to avoid misdiagnosis or unnecessary treatment. Implementing EHR software is one of the most effective ways to ensure that patient health and treatment data is readily available to medical professionals and seamlessly shared across departments and hospitals. It eliminates the need to run the same tests or collect the same data from a patient. Plus, patients can see their treatment plans, medication lists, and other important data.
Additionally, a typical VBP program should prioritize cost-efficiency in the provision of medical services. However, hospitals can’t ensure cost reduction for patients if they are simultaneously overspending due to poor visibility into budgets and expenses. Furthermore, if medical institutions frequently exceed their budgets, they may struggle to allocate necessary funds for technology upgrades or staff training, which affects quality improvement efforts.
Automating the purchasing process can save hospitals from challenges like out-of-control spending, exceeded budget limits, and unauthorized purchases. Procurement software helps medical institutions gain full visibility into hospital finances and find cost-saving opportunities while mitigating the risk of supply shortages.









